WHAT IS NALOXONE & HOW IT WORKS
WHAT IS NALOXONE?
Naloxone is a safe and effective opioid antagonist supported by peer-reviewed scientific literature dating back more than 50 years. Naloxone was first approved by the FDA in 1971 for the emergency treatment of known or suspected opioid overdose.
Naloxone’s approval in 1971 led to its increasingly widespread use as standard equipment in emergency medicine in the 1980s, before being distributed by harm reduction in the 1990s as part of their public health initiatives. Intranasal naloxone is a well-established way to provide safe, rapid, and effective opioid overdose reversals.
-
Both the Centers for Disease Control and Prevention (CDC) and local communities report that making naloxone more accessible saves lives.
-
The CDC reports that tens of thousands of lives have been saved since 1996.1 Naloxone has been shown to be successful in reversing opioid overdoses in 98.8% of cases.2
-
1 2. Wheeler, E., et al., Opioid Overdose Prevention Programs Providing Naloxone to Laypersons, 2014
-
2 Avetian, et al. (2018) DOI: 10.1080/03007995.2017.1334637
HOW NALOXONE WORKS
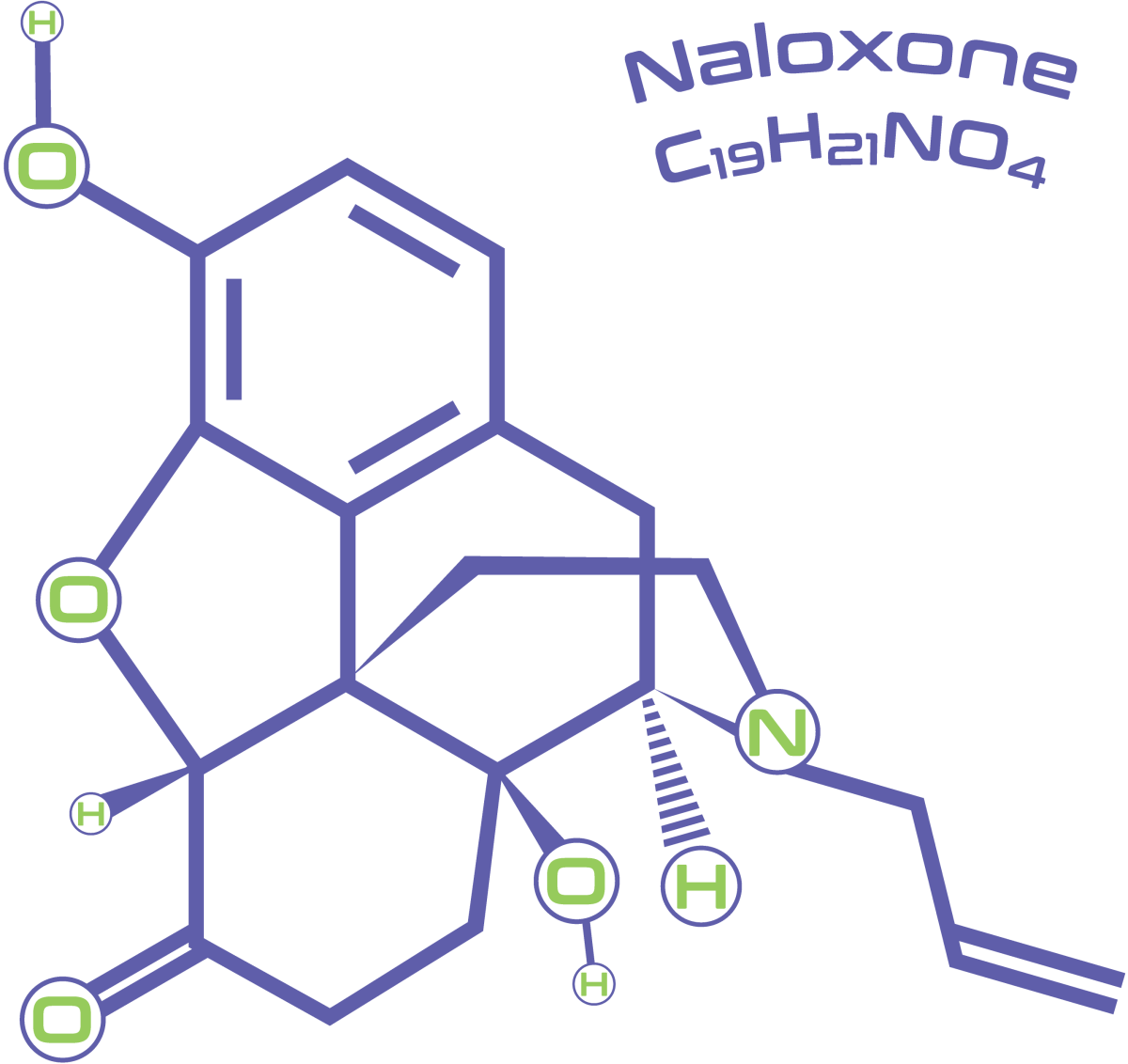
Naloxone is an opioid receptor antagonist, which means it binds to the opioid receptors in the nervous system and blocks or reverses the effects of the opioids that are being misused. In other words, naloxone competes with and pushes away the chemical signals from these opioids, restoring breathing and consciousness.
Literature supports the efficacy of naloxone in opioid overdose reversals broadly1 , including efficacy of both 2.0 mg2 and 4.0 mg intranasal (IN) naloxone formulations3 . Even 2.0 mg of intranasal naloxone given in various concentrations reverses opioid overdose in 74-82% of patients5,6 . Opioid-related overdose deaths are increasingly being driven by exposure to highly potent fentanyl and fentanyl analogs7,8 . A subset of opioid overdoses requires multiple administrations of 2.0 mg IN naloxone to successfully reverse. However, in a study of over 2166 patients who received naloxone in the field followed by paramedic support, 91% experienced complete resolution and reversal of symptoms after a single (mostly 2.0 mg; 51%) dose of IN naloxone and required no further advanced life support intervention. Only 9% required two or more doses of naloxone, and only 2.4% of patients required a third dose. Moreover, even in the context of illicitly manufactured fentanyl, studies have found no increases in the average number of naloxone doses used to reverse an overdose9 .
1 Wheeler, E., Jones, T.S., Gilbert, M.K., & Davidson, P.J. (2015). Opioid Overdose Prevention Programs Providing Naloxone to Laypersons — United States, 2014. Morbidity and Mortality Weekly Report, 64, 631 – 635.
2 McDonald, R., Lorch, U., Woodward, J., Bosse, B., Dooner, H., Mundin, G., Smith, K.J., & Strang, J. (2017). Pharmacokinetics of concentrated naloxone nasal spray for opioid overdose reversal: Phase I healthy volunteer study*. Addiction (Abingdon, England), 113, 484 – 493.
3 Avetian, G.K., Fiuty, P., Mazzella, S., Koppa, D., Heye, V., & Hebbar, P. (2018). Use of naloxone nasal spray 4 mg in the community setting: a survey of use by community organizations. Current Medical Research and Opinion, 34, 573 – 576.
4 https://www.samhsa.gov/resource/ebp/opioid-overdose-prevention-toolkit
5 Kelly, A., Kerr, D.C., Koutsogiannis, Z., Dietze, P.M., Patrick, I., & Walker, T. (2005). Randomised trial of intranasal versus intramuscular naloxone in prehospital treatment for suspected opioid overdose. Medical Journal of Australia, 182.
6 Kerr, D.C., Kelly, A., Dietze, P.M., Jolley, D., & Barger, B. (2009). Randomized controlled trial comparing the effectiveness and safety of intranasal and intramuscular naloxone for the treatment of suspected heroin overdose. Addiction, 104 12, 2067-74 .
7 O’Donnell, J., Tanz, L.J., Gladden, R.M., Davis, N.L., & Bitting, J. (2021). Trends in and Characteristics of Drug Overdose Deaths Involving Illicitly Manufactured Fentanyls — United States, 2019–2020. Morbidity and Mortality Weekly Report, 70, 1740 – 1746.
8 Rudd, R.A., Seth, P., David, F., & Scholl, L. (2016). Increases in Drug and Opioid-Involved Overdose Deaths – United States, 2010-2015. MMWR. Morbidity and mortality weekly report, 65 50-51, 1445-1452.
9 Bell et al., 2019
WHO SHOULD CARRY NALOXONE?
Friends and family of opioid users as well as Individuals that work, live or frequent areas where opioid misuse might be present.
HOW TO GET NALOXONE?
Today, naloxone is available in several ways:
- Prescription from your doctor.
- Over the counter at your local pharmacy or retail pharmacy chain.
- Free through community organization.
- National Organizations.
- Harm reduction programs, apply for access from Remedy Alliance/For the People here: Apply – Remedy Alliance / for the People (remedyallianceftp.org)
- People who use drugs, get supplier through NEXTDistro here: NEXT Distro
- Overdose first responders, find local resources here: Next Distro: Free Naloxone Access for Impacted Communities – Next Distro
SUPPORT GREATER ACCESS TO NALOXONE
Encourage your local and state authorities to pass laws and regulations promoting greater access to naloxone. Encourage them to dedicate funds and apply for federal grants that combat opioid misuse, including through increased distribution of naloxone. Spread the word about the importance
of having naloxone handy.
